Your ears don’t live in isolation. They’re plugged into your immune system, your metabolism, and even your stress response—all systems your gut microbiome helps tune. Early research suggests the tiny organisms in our intestines may influence how our ears age, how they handle noise and inflammation, and how we experience tinnitus. Intriguing? Absolutely. Settled science? Not yet. Here’s the state of the evidence, minus the hype, plus practical steps you can take now.
Wait—do the gut and the ear actually talk?
Indirectly, yes. Think of the gut as a chief advisor to your body’s defense and repair teams. The trillions of microbes in your intestines help train the immune system, produce signaling molecules, and shape inflammation throughout the body. Your inner ear—especially the cochlea and its stria vascularis—depends on a stable, low‑inflammation environment and a healthy blood supply. When systemic inflammation is up, or when the body’s stress systems are overactive, the ear can be more vulnerable.
A quick map of the highway
- Immune signaling: Gut microbes influence cytokines (immune messengers) that circulate everywhere—including near the ear’s blood–labyrinth barrier.
- Metabolites: Microbes produce short‑chain fatty acids (SCFAs) like butyrate and propionate that help maintain blood vessel and barrier health.
- Neural pathways: The gut–brain axis (including the vagus nerve) can modulate how the brain processes sound and stress, factors linked to tinnitus distress.
- Local neighbors: The ear, nose, and throat have their own microbiomes. Shifts in the nose/throat community can affect Eustachian tube function and middle‑ear health.
What the studies show so far
We’re early in this story. Most human studies are small or observational, and some findings come from animal models. Highlights:
- Tinnitus: Several small studies report different gut microbiome patterns in people with chronic tinnitus compared with controls. We don’t know if the microbiome changes cause tinnitus, result from it, or simply travel alongside shared factors like diet and stress. Mechanisms proposed include immune and stress‑axis modulation.
- Menière’s disease: Early work suggests people with Menière’s may show microbiome differences and heightened systemic inflammation. Whether microbiome‑targeted therapies help is unknown; rigorous trials are needed.
- Noise vulnerability: Animal studies indicate that altering gut microbes (for example, with certain antibiotics or dietary fibers) can change how ears respond to noise exposure—likely via inflammatory and vascular pathways. Translating this to humans will require careful clinical research.
- Otitis media (ear infections): In children, patterns in the nasopharyngeal microbiome are linked to recurrent ear infections. Some probiotic strains aimed at the mouth/throat show promise for reducing certain upper‑airway infections, but results are mixed and strain‑specific. Adult ear infections are less common; smoking exposure and allergies often play a larger role.
- Age‑related hearing: Aging shifts the gut microbiome and the immune system toward more inflammation (“inflammaging”). Observational studies have tied anti‑inflammatory dietary patterns (like Mediterranean‑style eating) to better hearing with age, but diet is a bundle of factors—not a microbiome silver bullet.
Bottom line: There’s a credible biologic story and some supportive data, but no microbiome‑based cure for hearing loss or tinnitus exists. Be wary of sweeping promises.
How could microbes influence ears? Plausible pathways
1) Inflammation and the blood–labyrinth barrier
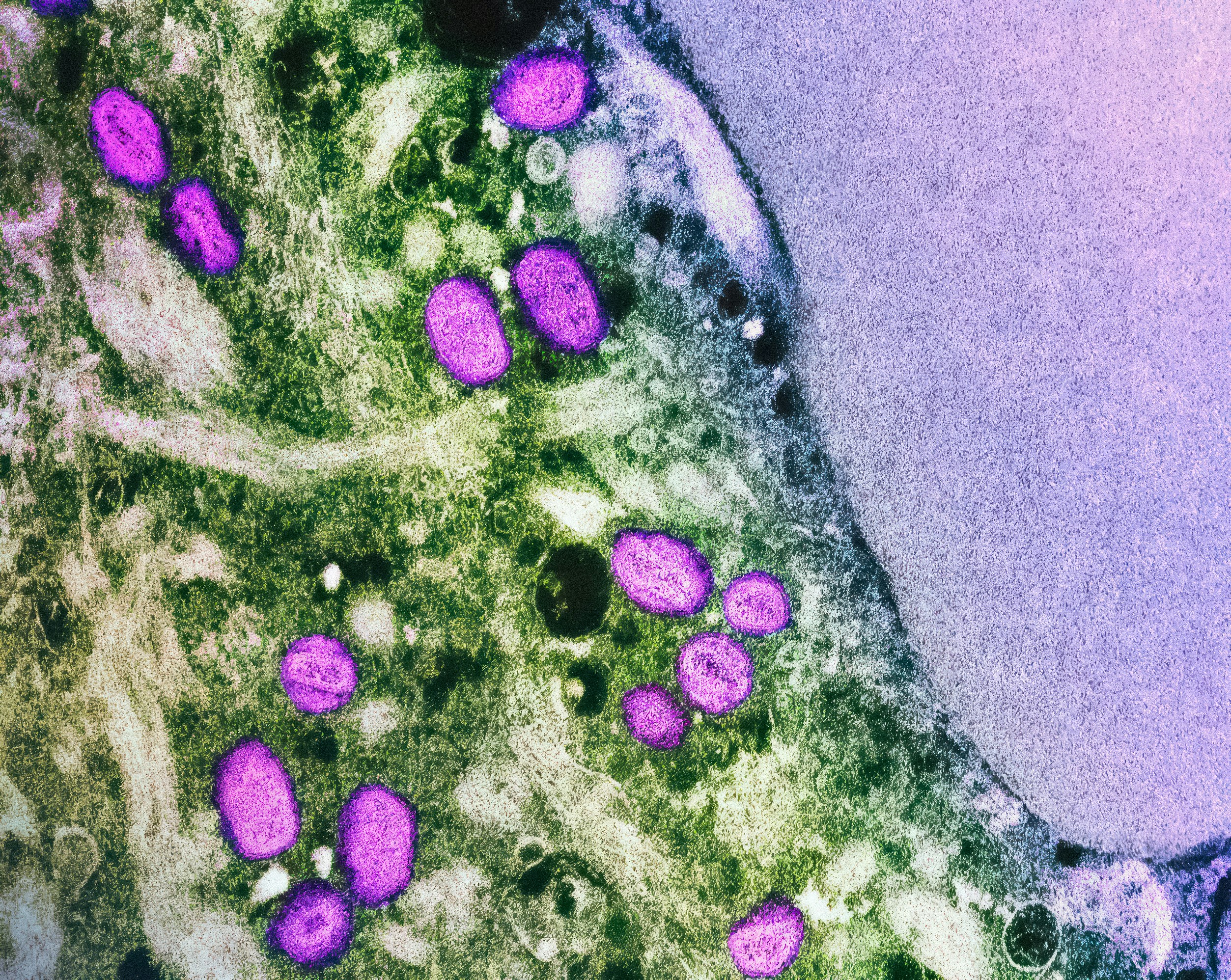
The inner ear relies on a protective barrier similar to the blood–brain barrier. When systemic inflammation rises, cytokines like TNF‑alpha and IL‑6 can alter vascular tone and barrier integrity, potentially stressing hair cells and auditory nerve synapses. Dysbiosis (an imbalanced gut microbiome) can fuel low‑grade inflammation through bacterial byproducts such as LPS (endotoxin).
2) Metabolites that nourish—and calm—tissues
SCFAs from fiber‑fermenting microbes help maintain blood vessel health, regulate immune cells, and may protect barriers. In animals, SCFAs can dampen harmful inflammation after noise or injury. Humans who eat more fiber and plant diversity tend to have more SCFA producers—one reason high‑fiber diets are broadly anti‑inflammatory.
3) Brain circuits, stress, and tinnitus perception
Tinnitus isn’t only about ear damage; it’s also about how the brain assigns meaning and priority to sound. The gut–brain axis affects mood, arousal, and stress reactivity—all of which shape tinnitus loudness and distress. Microbiome‑influencing habits that steady sleep, stress, and mood can help people cope better with tinnitus even if they don’t change the sound’s source.
4) The local neighborhood: nose, throat, and middle ear
Your Eustachian tubes ventilate the middle ear. Upper‑airway microbiome shifts can affect tube function and the risk of infections or fluid—especially in kids. Good airway health supports comfortable, pressure‑stable ears.
What this does not mean
- There’s no proven probiotic, cleanse, or supplement that cures tinnitus or restores hearing.
- Stool testing to “diagnose” ear problems is not recommended outside research.
- Do not stop medically necessary antibiotics. Some antibiotics are lifesaving; a few are ototoxic. Always discuss risks and alternatives with your clinician.
If you notice sudden hearing changes, ear pain, drainage, or one‑sided symptoms, seek prompt care. For ongoing hearing difficulty or tinnitus, an audiologist can establish a baseline and guide evidence‑based management.
Low‑risk habits that support both microbiome and ear health
None of these are ear cures. They’re solid, health‑forward moves that can lower systemic inflammation, support vascular health, and improve how you feel—and by extension, how you hear.
Build a fiber‑forward, plant‑rich plate
- Aim for 25–38 grams of fiber per day from beans, lentils, whole grains, vegetables, fruits, nuts, and seeds.
- Include fermented foods (yogurt with live cultures, kefir, kimchi, sauerkraut, tempeh) if tolerated. Start small if you’re not used to them.
- Lean toward a Mediterranean‑style pattern: olive oil, fish, legumes, leafy greens, colorful produce, modest dairy, minimal ultra‑processed foods.
Protect your sleep, move your body
- Adults generally need 7–9 hours of consistent, high‑quality sleep. Sleep regulates immune signaling and stress hormones that interact with tinnitus and inflammation.
- Get regular moderate activity (e.g., brisk walking, cycling, swimming). Exercise supports vascular health in the tiny blood vessels that feed the inner ear.
Be antibiotic‑smart
- Use antibiotics only when needed and as prescribed. This protects your microbiome and reduces resistance.
- Ask your clinician about the ear‑safety profile of any antibiotic if you already have hearing issues. Never stop prescribed meds without guidance.
Care for your airway
- Don’t smoke; avoid secondhand smoke. Both raise ear‑infection risk and inflame airways.
- Manage allergies with your clinician’s help to keep Eustachian tubes clear and comfortable.
- Nasal saline rinses can gently support nasal hygiene if you’re congested. Use sterile or distilled water and follow instructions.
Consider, don’t chase, probiotics
- If you’re curious, discuss targeted, evidence‑informed strains with your clinician—especially for recurrent throat infections or during/after antibiotics. Benefits are strain‑specific and modest; not all products are created equal.
- Focus first on dietary variety; it’s the main driver of a resilient microbiome.
When to see a professional
- Sudden hearing loss, a roaring ear, or new one‑sided tinnitus: urgent evaluation is essential.
- Persistent tinnitus, muffled hearing, or trouble understanding speech: book a hearing test with an audiologist. A clear picture of your hearing helps tailor solutions.
- Ear pain, drainage, fever, or repeated infections: see an ENT/primary care clinician.
Pros can help you rule out reversible causes, protect the hearing you have, and choose tools—hearing aids, sound therapy, counseling—that actually improve day‑to‑day life.
What to watch in the next few years
- Clinical trials testing whether diet or microbiome‑targeted therapies change tinnitus severity or hearing outcomes.
- Better mapping of ear‑specific immune responses and how systemic inflammation influences the blood–labyrinth barrier.
- Upper‑airway probiotic strategies for reducing recurrent ear problems in select groups.
We’re rooting for strong, sham‑controlled, adequately powered trials. Until then, keep your expectations realistic and your habits sustainable.
The bottom line
Your gut and your ears are connected through immune, metabolic, and neural pathways. Early research suggests the microbiome may influence hearing resilience and tinnitus—but we don’t have prescriptive protocols yet. The smartest moves today are timeless: steady sleep, regular movement, a fiber‑rich Mediterranean‑leaning diet, smart antibiotic use, and professional hearing care when symptoms arise. That’s a sound plan your ears—and your whole body—can get behind.
Further Reading
- From Gut to Cochlea: The Microbiome–Hearing Connection (What the Science Actually Says) (Research) - Your Heart, Your Hearing: The Cardiometabolic Link You Can’t Afford to Ignore (Research) - When Sleep Talks to Your Ears: Apnea, Insomnia, and the Circadian Cochlea (Research) - Sleep On It: How Nightly Rest Tunes Your Hearing and Calms Tinnitus (Research)Frequently Asked Questions
Can probiotics cure tinnitus?
No. There’s no evidence that any probiotic cures tinnitus. Some people feel better overall with certain strains, but benefits are modest and strain‑specific. If you want to try a probiotic, discuss options with your clinician and focus first on food‑based habits that support a healthy microbiome and lower stress, which can help with tinnitus coping.
Should I get a microbiome (stool) test for ear symptoms?
Not at this time. Stool tests can describe microbes but don’t diagnose ear conditions or reliably guide treatment for hearing or tinnitus. If you have ear symptoms, start with an audiologist for a hearing evaluation and your primary care clinician or an ENT for medical assessment.
Are antibiotics harmful to hearing because they change the microbiome?
Some antibiotics are potentially ototoxic, but many are not. Antibiotics can alter the microbiome, yet they’re often necessary and lifesaving. Always use them exactly as prescribed and ask your clinician about risks and ear‑safe options if you have hearing concerns. Don’t stop a prescribed antibiotic without medical advice.
Can diet really affect ear infections?
Diet alone won’t prevent every infection, but a nutrient‑dense, fiber‑rich pattern supports immune function and the microbiome. Avoiding tobacco smoke and managing allergies often matters more for ear pressure and infections. If ear infections are frequent, an ENT can assess anatomy, allergies, and other treatable drivers.