If voices sound muffled, you turn up the TV but still miss words, and oddly you hear people more easily in a noisy restaurant than in a quiet room—your stirrup bone (stapes) might be the quiet culprit. This is otosclerosis: a mechanical problem in the middle ear that’s frustrating, common in adults, and—good news—very treatable.
What exactly is otosclerosis?
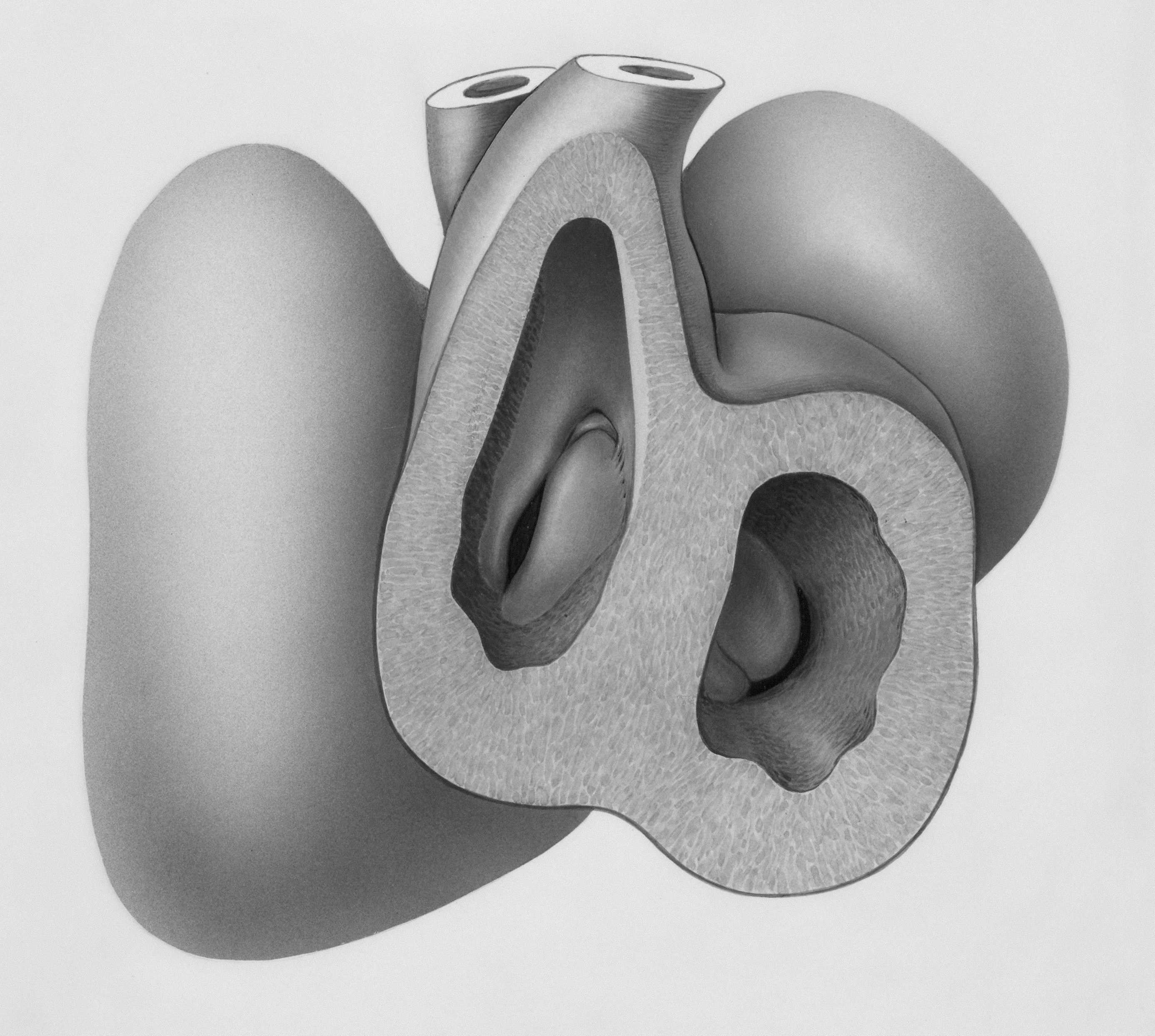
Otosclerosis is an abnormal remodeling of bone around the stapes, the tiny stirrup-shaped bone that transmits sound from your eardrum to your inner ear. When new bone grows and hardens around the stapes footplate, the bone can “stick,” reducing sound transmission. The result is typically a conductive hearing loss (sound can’t get in efficiently), sometimes with a sensorineural component if the inner ear is also affected (a mixed hearing loss).
It often starts in early to mid-adulthood and may run in families. It can affect one or both ears, and it often progresses gradually.
How otosclerosis feels in everyday life
- A slow, steady decline in hearing over months to years
- Paradoxically hearing speech better in noise than in quiet—called paracusis of Willis—because people naturally raise their voices in noisy settings
- Turning the TV up but still missing clarity in dialog
- Ringing or humming tinnitus
- Your own voice sounds booming or hollow (autophony)
- Ear fullness without pain or infection
Balance issues are less common with otosclerosis; significant spinning vertigo typically points to other causes and deserves prompt medical attention.
Why does it happen?
We don’t have one single cause, but research points to:
- Genetics: Otosclerosis often runs in families with variable expression.
- Bone remodeling biology: The middle ear’s delicate bony capsule undergoes abnormal turnover in specific spots, especially near the stapes footplate.
- Hormonal influence: Some people notice changes during pregnancy or hormonal shifts.
- Viral and immune factors: Historic links to measles have been explored; modern vaccination has reduced measles but not eliminated otosclerosis. Autoimmune mechanisms are also under study.
Getting the right diagnosis (and ruling out look-alikes)
Because the ear canal and eardrum often look normal, otosclerosis can masquerade as “just wax” or “just getting older.” A targeted evaluation makes the difference.
Start with an audiologist
- Pure-tone audiogram: Otosclerosis classically shows an air-bone gap (sound blocked in the middle ear). Some people show a “Carhart notch” (a dip around 2 kHz).
- Speech testing: Word recognition is often relatively good once sound is loud enough, supporting a conductive component.
- Tympanometry and acoustic reflexes: The eardrum movement often looks normal, but acoustic reflexes may be absent, hinting at stapes fixation.
Then an ear physician (ENT/otologist)
- Microscope exam to rule out eardrum or ear canal problems.
- Imaging (CT) only when needed to clarify anatomy or surgical planning.
Other conditions can cause similar symptoms, including earwax buildup, fluid from Eustachian tube dysfunction, ossicular chain problems, or congenital fixation. That’s why a team approach—audiologist plus ENT—is ideal.
If you notice sudden hearing loss over hours or days, that’s different. Treat it as an urgent medical issue and contact an ENT promptly.
Your treatment options—clear, practical, and personal
There are three main pathways. The best one is the one that fits your hearing, health, and lifestyle today.
1) Watchful waiting plus protection
- If hearing is mild and your communication needs are minimal, periodic hearing tests can track progression.
- Protect your ears from loud noise (concerts, power tools) to preserve inner-ear health.
- Healthy sleep, exercise, and heart health support overall ear circulation.
2) Hearing aids (powerful for conductive loss)
Because your inner ear may still be quite capable, hearing aids often deliver excellent clarity by simply overcoming the mechanical blockage.
- Why they work so well: Conductive losses keep sound from reaching the inner ear; amplification restores it.
- Styles: Behind-the-ear receiver-in-canal (RIC) or custom in-the-ear. A custom earmold can help deliver power comfortably and reduce feedback.
- Features to prioritize: Directional microphones for speech-in-noise, feedback control, and good physical retention.
- Follow-up matters: Expect a few visits for fine-tuning as your brain adapts to clearer sound.
Many people choose hearing aids first—even if they’re good surgical candidates—because it’s reversible, low risk, and can be fit quickly.
3) Stapes surgery (tiny fix for a tiny bone)
Two closely related procedures can “unstick” the system:
- Stapedotomy: A tiny opening is made in the fixed stapes footplate and a micro-prosthesis (piston) connects the incus to the inner ear through that opening.
- Stapedectomy: Removal of part or all of the stapes footplate with placement of a prosthesis. Many surgeons now prefer stapedotomy due to control and safety.
What to expect:
- Usually outpatient with local or general anesthesia.
- Hearing often improves within days to weeks as swelling subsides.
- Success rates are high for closing the air-bone gap, commonly in the 80–90% range.
- Risks include temporary dizziness, taste changes (the chorda tympani nerve runs nearby), and in rare cases a permanent inner-ear hearing loss.
How to decide: If your audiogram shows a sizeable air-bone gap, your eardrum and middle ear look healthy, and your overall health is good, you’re likely a candidate. Many surgeons operate on the worse ear first and wait several months before considering the other side.
What surgery doesn’t do: It doesn’t stop all future change in the ear. Some people still use a hearing aid after surgery—usually at a much lower gain—especially if there’s an inner-ear component. That’s okay; the combo can be life-changing.
Pregnancy, hormones, and hearing
Some individuals with otosclerosis notice progression during pregnancy or hormonal shifts. If you’re planning pregnancy or are pregnant and noticing changes in hearing or tinnitus, schedule an audiogram. Surgery is typically postponed until after delivery; hearing aids can bridge the gap during pregnancy.
Everyday habits that support better hearing
- Noise protection: Use high-fidelity earplugs at concerts and proper protection for tools and yardwork. Protecting your inner ear reduces the chance of a mixed loss.
- Heart-healthy lifestyle: What’s good for your blood vessels is good for your cochlea—think movement, balanced nutrition, and not smoking.
- Regular check-ins: If you’ve been told you have otosclerosis, get periodic hearing tests to spot change early.
Myths and facts
- “Hearing aids will make my ears lazy.” False. They provide needed input; your brain does the rest.
- “Surgery is a last resort.” Not necessarily. For the right candidate, stapes surgery is a first-line, highly effective option. It’s about your goals and comfort.
- “Fluoride pills cure otosclerosis.” Evidence for medical therapy is limited and not routinely recommended. Discuss any medication claims with your ENT.
- “If it’s genetic, nothing can help.” Genetics may influence cause, but your options—hearing aids and surgery—are very effective.
Making your decision: a simple framework
Ask yourself:
- How much is hearing loss affecting my work, relationships, and energy?
- Am I comfortable trying hearing aids first, or do I prefer a one-time surgical fix if I’m a candidate?
- Do I have support for post-op recovery if I choose surgery?
And ask your care team:
- Is my loss mostly conductive? What’s my air-bone gap today?
- What outcomes do you expect for me with hearing aids vs. surgery?
- How many stapes surgeries do you perform each year, and what are your outcomes?
- What’s the plan if I still need a hearing aid after surgery?
A collaborative conversation with your audiologist and ENT/otologist will quickly clarify the best next step for you.
Costs and coverage (quick glance)
- Hearing aids: Coverage varies widely; some plans or employer benefits help. Ask about trial periods, warranties, and follow-up visits.
- Stapes surgery: Often covered when medically indicated. Pre-authorization is common. Ask about surgeon fees, facility fees, anesthesia, and post-op visits.
Quick self-check (not a diagnosis)
- Do you hear speech more clearly in noisy places than quiet ones?
- Have family members started mumbling “suspiciously” over the past year?
- Does your hearing test mention an air-bone gap or absent acoustic reflexes?
If you’re nodding “yes,” consider booking with an audiologist for a comprehensive hearing evaluation and an ENT for a medical exam. The earlier you clarify what’s going on, the more options you have—and the easier communication gets.
The bottom line
Otosclerosis is a mechanical hearing problem with real, effective solutions. Whether you choose precise amplification, elegant microsurgery, or a combination, you can expect conversations to feel easier, listening to cost less energy, and life to sound more like you remember. Reach out to a licensed audiologist and an experienced ENT/otologist to map your next step.
Further Reading
- Otosclerosis Treatment: Stapedotomy or Hearing Aids—How to Choose (Treatment) - When Sound Fades Overnight: The Hearing Emergency You Should Never Ignore (Hearing Loss) - Sudden Hearing Loss? Don’t Wait—The 72‑Hour Window That Can Save Your Hearing (Hearing Loss) - Tinnitus, Trained: CBT, Sound Therapy, and Habits That Actually Help (Treatment)Frequently Asked Questions
How is otosclerosis different from fluid or ear infections?
Otosclerosis is a mechanical fixation of the stapes bone, often with a normal-looking eardrum and no pain. Fluid or infections typically cause earache, pressure, or fever and show abnormal eardrum findings. An audiogram helps distinguish them: otosclerosis shows a conductive hearing loss with an air-bone gap and often absent acoustic reflexes.
What is the success rate of stapes surgery, and what is recovery like?
Most candidates experience a significant improvement in hearing, with closure of the air-bone gap in roughly 80–90% of cases. Surgery is usually outpatient. You may feel off-balance for a few days and taste changes can occur temporarily. Many people notice clearer hearing within days to weeks as healing progresses. Discuss your individual risks and expected outcomes with your surgeon.
Will I still need a hearing aid after surgery?
Some people no longer need a device, while others benefit from a hearing aid at lower levels, especially if there’s a sensorineural component. Think of surgery as restoring the mechanical pathway; if the inner ear has some wear-and-tear, light amplification can polish the result.
Can otosclerosis worsen during pregnancy?
Hearing changes during pregnancy have been reported in some people with otosclerosis. If you’re pregnant and notice new or worsening hearing loss or tinnitus, get a hearing test and consult an ENT. Hearing aids are safe to use during pregnancy, and surgery is typically considered after delivery.