What if we could fix a broken hearing gene or coax the inner ear to regrow its delicate sensors? That’s no longer just sci‑fi. Early human trials are now testing gene therapy for specific genetic hearing losses, and scientists are refining strategies to regenerate or repair inner‑ear cells. It’s exciting—and complicated. Here’s your clear, grounded tour of what’s real today, what’s coming, and how to navigate the hope without the hype.
The quick take
- Some forms of congenital sensorineural hearing loss—especially those caused by single‑gene mutations like OTOF—are the earliest candidates for gene therapy.
- Initial human studies have shown promising signs of restored auditory responses in certain children with OTOF‑related auditory neuropathy, but results vary and longer follow‑up is needed.
- Hair‑cell regeneration in humans remains experimental; earlier drug programs stumbled, but next‑gen approaches are in preclinical development.
- Most adult age‑related or noise‑induced hearing loss will not be fixed by gene therapy soon. Don’t wait—today’s hearing care (hearing aids, cochlear implants, assistive mics, therapy) changes lives now.
- If you suspect a genetic cause, ask an audiologist or ENT about genetic testing and research registries; this is the gateway to relevant trials.
Why your genes matter to your ears
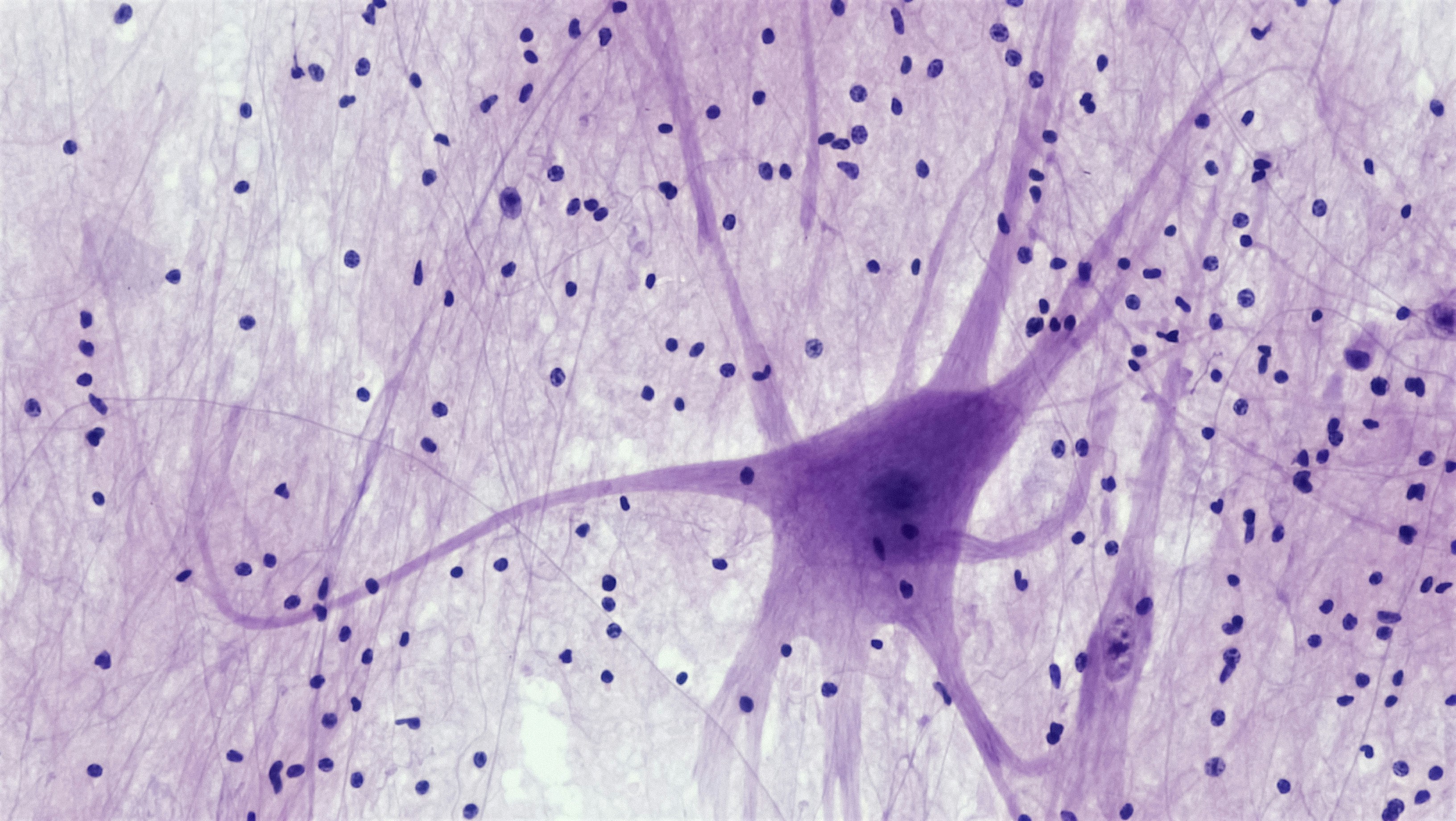
Your inner ear (cochlea) translates tiny vibrations into the electrical language your brain understands. The stars of this show are hair cells and the synapses that connect them to the hearing nerve. Dozens of genes choreograph this ballet—building structures, regulating ions, releasing neurotransmitters.
When one of these genes is altered, the result can be sensorineural hearing loss. For example, OTOF (otoferlin) is essential for fast, precise release of neurotransmitters at the inner hair cell synapse. Children born with biallelic OTOF variants often have auditory neuropathy: the ear can detect sound, but signals don’t fire properly to the nerve.
That’s exactly the kind of problem gene therapy can target: fix or replace a single faulty instruction so the system can work again.
Two big strategies: fix the gene or rebuild the parts
1) Gene replacement in the cochlea
Most current clinical trials use harmless viral “envelopes” (often AAV—adeno‑associated virus) to deliver a healthy copy of a gene to inner‑ear cells. Surgeons place the vector through the middle ear to the round window, allowing it to diffuse into the cochlea. The aim: get enough cells producing the needed protein to restore function.
Early human trials focus on OTOF because it causes a well‑defined, stable hearing loss and has a clear cellular target. Importantly, the hair cells are usually present; what’s missing is the chemical handshake with the nerve. Replace the handshake, and you might restore signal.
2) Gene editing and base editing
In the lab, CRISPR‑based tools can repair specific DNA typos or silence toxic versions of a gene. Base editors and prime editors offer even finer control. Several teams have corrected hearing‑related mutations in animal models. But editing is not yet in mainstream human ear trials; researchers are working to ensure precision, safety, and durable benefit without off‑target effects.
3) Hair‑cell regeneration and synapse repair
Another line of attack tries to turn supporting cells into new hair cells, often by switching on developmental programs (think ATOH1) or by nudging cell division. So far, early human attempts to regrow or rescue hair cells after common acquired hearing loss haven’t succeeded clinically. Some programs halted after negative trials, but the biology keeps advancing: better delivery, timing, and combo therapies (for example, regrowing hair cells plus repairing their synapses) are being explored in animals.
What early human studies are showing
The headline: a small number of children with OTOF‑related auditory neuropathy who received inner‑ear gene therapy have shown objective improvements on tests like the auditory brainstem response (ABR) and measurable hearing thresholds, with early reports of sound awareness and speech progress. Many protocols treat one ear first to assess safety and benefit.
That’s encouraging, but we need to keep our feet on the ground. Key unknowns include:
- Durability: How long will benefit last from a single dose?
- Consistency: Will all children with OTOF variants respond, and to what degree?
- Timing: Is there an age window where the brain is most ready to use the restored signal?
- Safety and re‑dosing: AAV can trigger immune responses that complicate future dosing.
Other gene targets are entering or preparing for trials, but each condition has unique challenges: gene size (some won’t fit in standard AAV), which cells must be reached, and whether those cells still exist in the ear by the time of treatment.
Who may benefit first—and how to find out
Gene therapy is most likely to help individuals who have:
- A well‑characterized, single‑gene cause of hearing loss (e.g., OTOF) confirmed by genetic testing.
- Intact inner ear structures (hair cells present) but a known molecular defect.
- Hearing loss identified early in life, when auditory pathways are still highly plastic.
If your child has auditory neuropathy or congenital sensorineural hearing loss, ask your audiologist or ENT about genetic testing. A positive, actionable result places you on the radar for relevant studies and informs counseling, even if you never join a trial.
Practical steps:
- Request a referral to a genetic counselor and discuss a comprehensive hearing‑loss panel.
- Enroll in registry efforts or natural history studies if offered—these help accelerate research and keep families informed.
- Search ClinicalTrials.gov using terms like “OTOF,” “AAV,” or “inner ear gene therapy,” and share any candidates with your care team.
Gentle reminder: trials have strict inclusion criteria for safety and scientific clarity. If you don’t qualify, it’s not a value judgment—your care still matters, and there are many effective options today.
How these treatments are delivered (and the risks)
Most inner‑ear gene therapies are administered in the operating room using a tiny catheter placed near the round window of the cochlea. It’s delicate but familiar territory for otologic surgeons. As with any ear surgery, potential risks include infection, dizziness, taste disturbance, or even worsened hearing in rare cases. Teams monitor closely with hearing tests and imaging, starting with one ear when appropriate.
Ask your ENT or otologist to walk you through center experience, anesthesia plans, and recovery timelines if you’re considering a study.
What about adults with age‑related or noise‑induced hearing loss?
This is the question we hear daily. For now, gene therapy is unlikely to help most adults with presbycusis (age‑related hearing loss) or long‑standing noise‑induced damage. These conditions typically involve many pathways: cumulative hair‑cell loss, synapse damage, metabolic changes, and central processing shifts. There isn’t a single gene “fix.”
But that doesn’t mean you’re stuck. Today’s care is powerful:
- Modern hearing aids with directional mics, frequency lowering, Bluetooth streaming, and personalized fitting make conversations easier—and safer listening encourages brain health.
- Cochlear implants can provide excellent speech understanding for those who no longer benefit from hearing aids.
- Assistive microphones and speech‑to‑text tech de‑stress group settings.
- Tinnitus therapies (sound therapy, CBT approaches, and emerging neuromodulation) reduce distress and improve sleep.
If you’re struggling, book a hearing evaluation with an audiologist. The best “future‑proofing” is hearing well now.
Where hair‑cell regeneration stands
Can we regrow the inner ear’s microphones? In mammals, adult hair cells don’t naturally regenerate. Drug programs aimed at re‑awakening that capacity have not yet shown clear benefit in people with common acquired hearing loss. Scientists are learning from those results, refining:
- Which supporting cells to target and when
- How to rebuild hair‑cell synapses as well as cells
- Whether combined approaches (regeneration + neurotrophins) are needed
Bottom line: hair‑cell regeneration is a marathon, not a sprint. It’s an area to watch, but not to plan your care around today.
Open questions researchers are racing to answer
- Durability: Will a single gene‑therapy dose support hearing for years, and can it be safely repeated?
- Precision delivery: Can we reach just the right cells in the intricate spiral of the cochlea?
- Immune responses: How do we minimize unwanted immunity to viral vectors?
- Neural plasticity: If hearing is restored later, how well will the brain adapt? Will children need intensive auditory therapy afterward?
What you can do now while the future matures
- Protect your hearing: keep volumes in the safe zone and use hearing protection in loud settings.
- Manage health basics: cardiovascular fitness, blood pressure, and diabetes care all support inner‑ear resilience.
- Audit your medicines with your clinicians if you have concerns about ototoxicity—never stop a prescribed drug on your own.
- Stay connected: If genetic hearing loss is in your family, consider counseling and keep an eye on reputable trial listings with your care team.
Curious about whether your hearing history suggests genetics? An audiologist can review your audiogram pattern, family history, and age of onset and help coordinate next steps. Your ears deserve a personalized plan.
Follow the science, not the headlines
We’re living through the first real tests of inner‑ear gene therapy in people. That’s enormous. It’s also early. Celebrate the progress, advocate for access and safety, and keep working with your local audiology and ENT team to hear your best today—because better hearing now supports your brain, your relationships, and your future.
If you’re considering research participation, bring an audiologist or ENT into the conversation early. They’ll help you understand eligibility, risks, and alternatives—and cheer you on, whichever path you choose.
Further Reading
- Hearing Damage, Measured in a Drop: The Emerging Science of Ear Biomarkers (Research) - Can We Regrow Hearing? Inside Hair-Cell, Synapse, and Gene Therapies Now (Research) - Hidden Hearing Loss Is Real: Why a Normal Audiogram Can Still Leave You Struggling in Noise (Research) - Can We Rebuild Hearing? The Real State of Hair Cell Regrowth and Gene Therapy (Research)Frequently Asked Questions
Will gene therapy fix age‑related or noise‑induced hearing loss soon?
Unlikely in the near term. Most adult sensorineural hearing loss involves multiple pathways and cumulative damage, not a single gene error. Current gene therapies focus on specific monogenic conditions, often in children. Don’t wait—today’s hearing aids, cochlear implants, assistive microphones, and therapy can dramatically improve communication and quality of life.
Is inner‑ear gene therapy safe for kids?
Early studies suggest it can be delivered safely in specialized centers, typically to one ear first. As with any ear surgery and viral‑vector therapy, risks include infection, dizziness, taste disturbance, immune responses, or changes in hearing. Families should review potential benefits and risks with a pediatric otologist, audiologist, and genetic counselor.
If my child already has a cochlear implant, could they still be eligible for gene therapy?
Eligibility is trial‑specific. Some protocols exclude previously implanted ears, while others may allow treatment in the non‑implanted ear. Your existing implant does not prevent you from exploring research, but it’s important to discuss realistic goals and risks with your care team.
How do I know if our hearing loss is genetic?
Patterns like early onset, family history, and certain audiogram shapes can hint at genetics, but the only way to know is through genetic testing. Ask your audiologist or ENT for a referral to a genetic counselor and a comprehensive hearing‑loss gene panel. Results can guide care and determine trial eligibility.